Reposting from
Europe’s Coronavirus Fate Is Already Sealed
One reason Britain and Italy are struggling: Their medical systems are too dependent on government. by Joseph Sternberg.
Scientists around the world have worked overtime to get a handle on COVID-19, yet one great unknown remains. We still don’t know for sure whether this is only a medical crisis, or also a medical system crisis.
The distinction matters for the novel coronavirus for the same reason it matters for other “natural disasters” that aren’t entirely natural. It is now widely understood that famines arise from local political failures in the trade and distribution of abundant global food supplies, not from local crop failures. Floods devastate communities not because the local rivers are unusually watery but because poor zoning and subsidized flood insurance encourage people to build homes in flood plains.
This is the context for a conspicuous feature of COVID-19: It is not untreatable, but many health systems are struggling to deliver effective treatment. Nowhere is this more so right now than in Italy, where nightmarish reports are emerging from hospitals in the hardest-hit areas.
Doctors in Italy know what to do to treat severe cases, such as using ventilators in intensive-care units. But hospitals lack the beds and equipment for the influx of patients, and Italy doesn’t have enough doctors even to make the attempt. Ill patients languish in hospital corridors for want of beds, recovering patients are rushed out the door as quickly as possible, and exhausted (and sometimes sick) doctors and nurses can’t even muster the energy to throw up their hands in despair.
Is this more a result of the severity of COVID-19, or of long-term failures to invest in the Italian health-care system? One starts to suspect the latter.
Italy lags behind other large European countries in provision of acute-care hospital beds, furnishing 2.62 of them per 1,000 residents as of 2016, according to the Organization for Economic Cooperation and Development. In Germany it’s 6.06 and in France and the Netherlands it’s 3.15 and 3 respectively. That year, Italy devoted around $913 per capita to inpatient acute and rehabilitative care, compared with $1,338 in France, $1,506 in Germany, and $1,732 in the U.S.
U.K. policy makers understand what such analyses portend — because underinvestment in Britain’s creaking health-care system is even worse. The U.K. spent the princely sum of $901.70 per capita on acute care in 2016, according to the OECD. British data don’t distinguish acute-care beds, but a comparison of available beds overall isn’t any more favorable to the U.K. (or to Italy). In 2017, when Germany provided 8 beds per 1,000 residents and France offered 5.98, Italy managed 3.18, and the U.K. only 2.54.
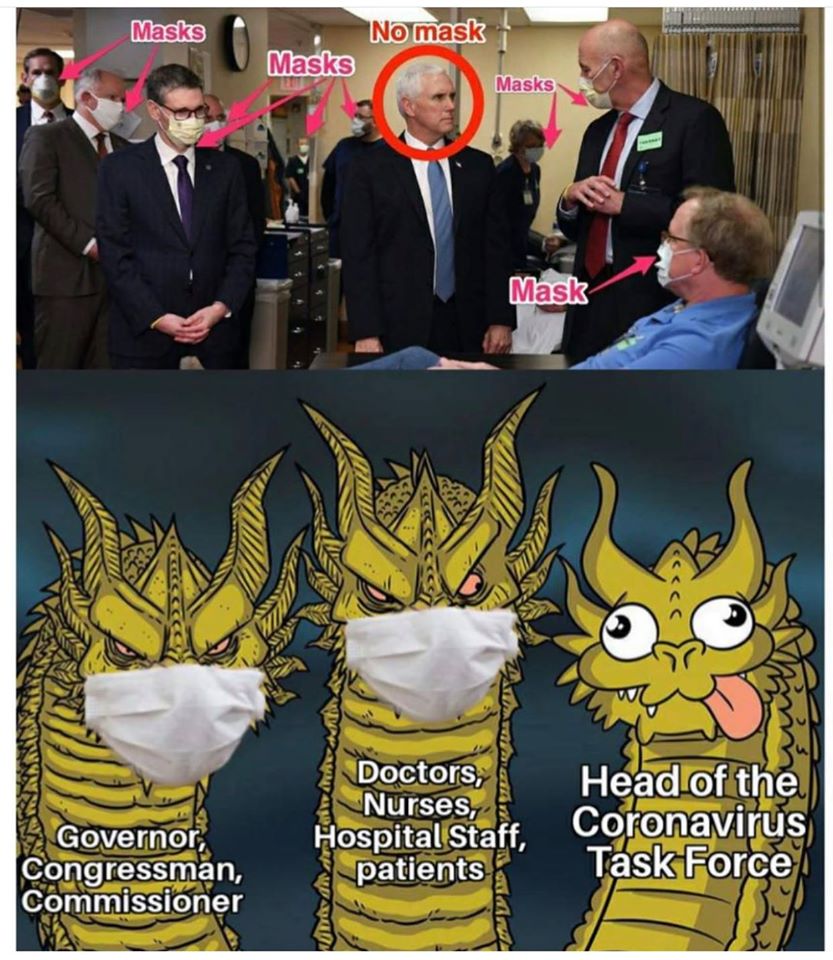
As a result, British authorities have adopted a very specific policy goal in their approach to COVID-19. The aim is not to prevent the virus’s spread through the general population, which is a foregone conclusion. Rather, the name of the game is delay. British authorities are desperate to hold off on a mass outbreak until the socialized National Health Service has recovered from its chronic winter crisis.
That’s right, the NHS, which now will have to cope with a new and fast-moving respiratory illness, already falls to pieces every year with the normal ebb and flow of cold-weather ailments. Each winter crisis becomes a bit more acute, and this year was no exception. As of December, only 80% of emergency-room patients were treated within four hours of arrival, down from 84% in the depths of the previous two winters.
What accounts for these divergences in health-care resources requires more study than a single newspaper column can provide, but a few early hints emerge. One is the observation that the U.K. and Italy are significantly more dependent on direct government financing of health-care than is France or Germany.
Government accounted for 79% of total health-care spending in the U.K. in 2017, according to Eurostat, and 74% in Italy. Germany and France both rely on compulsory insurance schemes with varying degrees of subsidy and government meddling, but outright government expenditure amounts to only 6% of total health spending in Germany and 5% in France. COVID-19 in this sense is a test of how much one trusts central health planners to make wise long-term decisions that boost resilience in the face of unusual dangers.
This story is food for thought for voters inclined to skepticism over the wisdom or efficacy of their politicians’ responses to the crisis. Those same politicians already have made decisions that may seal a country’s coronavirus fate, and it won’t have anything to do with quarantines or restrictions on travel or large gatherings. Rather, the important choices may have already come in the guise of technocratic health spending and investment decisions made largely out of public view over many years. How lucky do Europeans feel?