The following paragraphs are just random thoughts and articles that might shed some light on the disease that is lichen planus (thinking too some variants of the disease like hypertrophic lichen planus and lichenoid drug-induced eruptions (which i would rename lichenoid like dermatoses) with various environmental triggers. I found a relatively old publication in the 1990s that clearly felt environmental factors were important in LP, but with passing years and changes in research-topic “runway-fashions” the environmental influence gets less attention.
Reading an article on histologic distinctions between lichen planus and lichenoid drub-induced dermatitis (link reference given previously) I think it is a perfect description of what I have experienced and a perfect expression of the gene environment interactions that go along with other cases where the immune system decides to make massive amounts of antibodies to a “wrong thing” — as the online definition of anamnestic states so beautifully “an enhanced reaction of the body’s immune system to an antigen that is related to an antigen previously encountered”
I cant wait (but am apparently going to wait a long time) for my condition to clear so i can go back and test if my assumption about mortar, grout, cement, concrete and additives are the “guilty-by-association antigens” that cause this disease.
AND here is a new tack. duh, i should have thought this up a long time ago. I have been slightly aware that potatoes (not sweet potatoes or yams) might cause an increase in itchiness of my lichen planus spots. I did cut out potatoes and peppers for a while, but then on June 6 2018 (that is about 9 months into the flare up of this disease in my) I went back to eating peppers tomatoes and potatoes (all nightshade family members). Yesterday i cut out potatoes again…. so Then i googled, nightshade plants and immune response and find again, what i knew once, that those have “lectins”. Make the connection here. Lung cells (in particular, alveolar type II cells) secrete surfactant protein A… the latter is named a surfactant protein, and it does in fact participate in the formation of tubular myelin in the alveolar spaces but one can live just fine and had sufficient lung function WITHOUT surfactant A. That said, there are immune consequences because surfactant A is a C-type lectin (lung reaction allergens) and
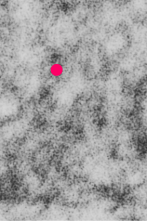
“Antigen-presenting cells can capture antigens that are deposited in the skin, including vaccines given subcutaneously” (Flatcher et al, J. Invest. Derm. 2010 Mar;130(3):755-62. doi: 10.1038/jid.2009.343).
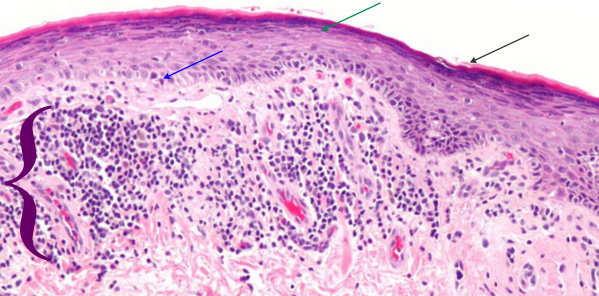
Aside: shame on whomever called lichen planus a benign situation… ha ha.. clearly never had it. Bless the person who describes the causes of lichen planus as “undefined” because clearly there is a cause, and likely a multitude of causes, and I add, many are going to be environmental… mistaken identity immunity, or inappropriate immune responses. Bless the guy who mentions adhesion molecules in this disease…. i have no clue how the extracellular adhesion molecules in epidermis can tell the difference between “sheer” (rubbing) and patting (e.g. patting dry an area of lichen planus eruptions) but the cells know… a tiny bit of sheer tension and it triggers highly intense itching. It only took one google search to find this article which actually mentions extracellular adhesion molecules in Pemphigus, so this is not far from responses in lichen planus.
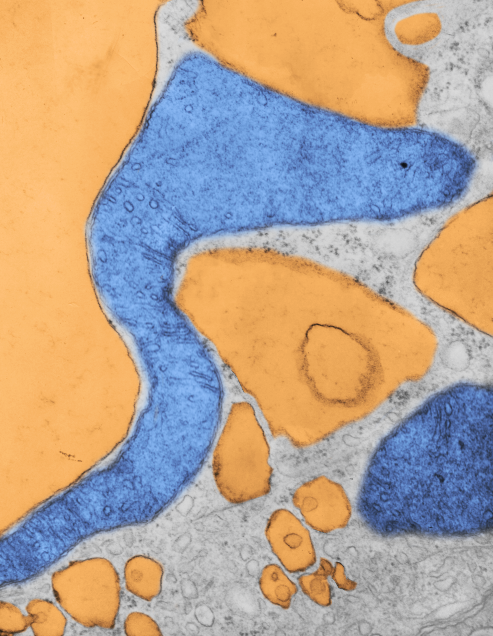
And another article here which describes roles for langerhans cells… goodness, maybe direct access of environmental materials (as in my case, cement, mortar, thinset mortar grout, and whatever was present on acorn debris thrown up into my shins from my lawnmower) was opsonized by the langerin (C-type lectin) surface protein in my epidermal langerhans cells… ha ha… so much fun to learn this stuff… and to suppose what processes might have occurred.